Osteoporosis and Osteopenia: What You Need to Know About Bone Health

Maintaining optimal bone health is crucial for overall well-being and quality of life. Our bones do naturally get weaker as we age. In this article, we dive into the significance of bone health, what osteoporosis and osteopenia are, and everything you need to know about your bone health. By understanding the essential role of bone health and adopting preventive strategies, individuals can take proactive steps towards safeguarding their skeletal well-being and enjoying an active lifestyle.
What is Osteoporosis and Osteopenia?
Osteoporosis is defined by the World Health Organisation (WHO) as a disease characterized by low bone density and a deterioration of the bone tissue leading to bone fragility and as a consequence, increased risk of fracture. It is typically known as a “silent” disease because it is often not diagnosed until after a broken bone (fracture) has occurred following a minor incident.
Osteopenia is a lower than normal bone density. This means that that your bones are classified as weaker (or less dense) than normal, but not quite as weak as those with osteoporosis. It is considered a “warning” zone for action to halt the loss or even to improve bone density.
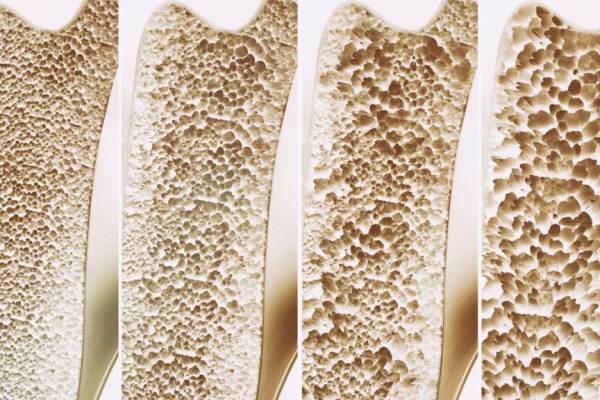
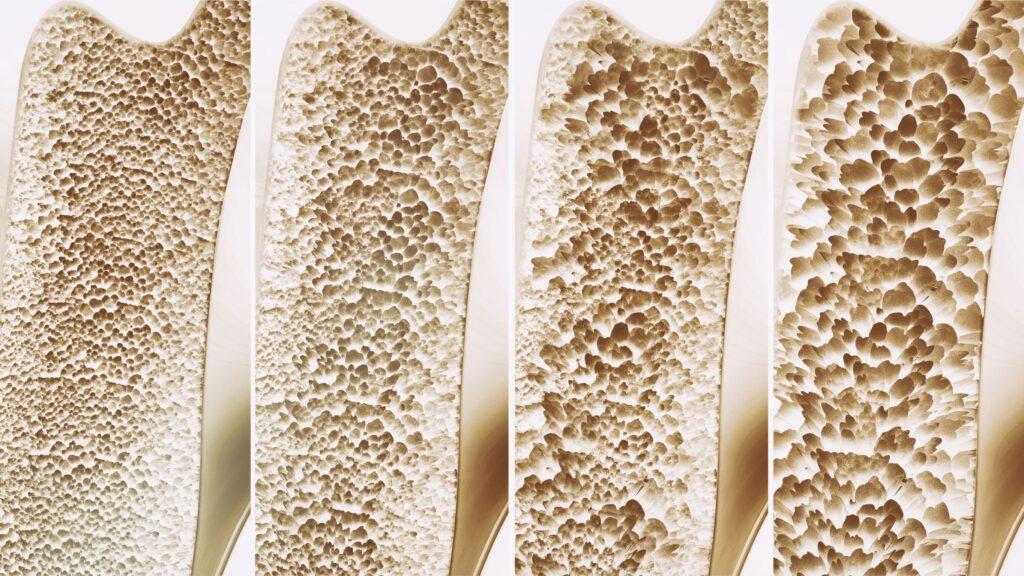
Osteoporosis is characterized by low bone density leading to bone fragility and as a consequence, an increased risk of fracture.
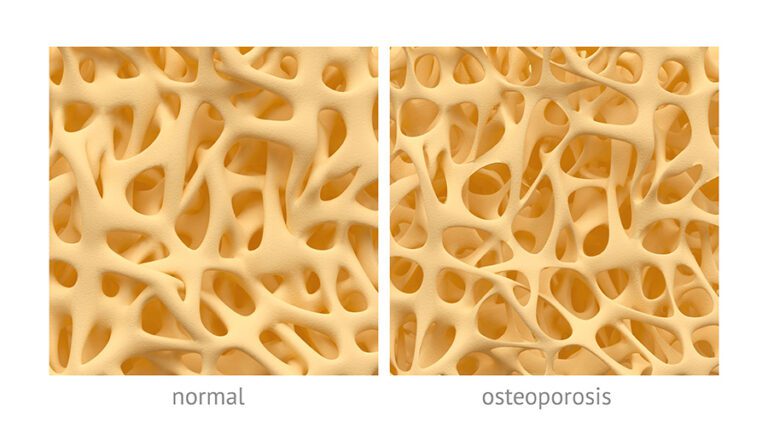
A comparison of normal bone density versus low bone density
Key Statistics:
Osteoporosis affects around 200 million women worldwide
Menopause increases the risk of developing osteoporosis
Bones become less dense as we age leading to an increased risk of bone fracture
Most common bones to break are the wrist, hip, and spine
1 in 3 women over age 50 will experience osteoporosis fractures worldwide
1 in 5 men aged over 50 will have low bone density. For Asian and Caucasian men, the statistics is 1 in 3 men
Why is Bone Health Important For Us?
Maintaining good bone health is crucial for several reasons. Firstly, it helps prevent fractures, which become more common and debilitating with age. Strong bones provide structural support, enabling mobility and independence in performing daily activities. With good bone health and density, individuals can preserve their quality of life, avoiding chronic pain and limited mobility.
Unfortunately, osteoporosis is fairly common in Hong Kong and research has shown that there has been a 73% increase in the annual number of hip fractures requiring surgery over the last 20 years (Man et al, 2019). Fragile fractures (falls from standing height) incur both an economic and personal cost to the community. Low bone density, osteoporosis and osteopenia will affect your risk of fractures, injury, pain, quality of life and rehabilitation time.
Research by the Osteoporosis Society of Hong Kong predicts that the number of hip fractures caused by osteoporosis alone will triple over the next 30 years. As Hong Kong has a rapidly aging population with a relatively high life expectancy, they urge people to be tested and to start appropriate “healthy bones” interventions early.

Osteoporosis is a ‘silent disease’ because most people are diagnosed with osteoporosis only after they suffer a fracture after a minor fall: a “fragility” fracture.
What Happens to Our Bone Health as We Age?
Bone growth is rapid during childhood and adolescence and we reach a peak bone mass around the age of 30. After that there is a steady rate of age-related loss of bone for both men and women. For women, there is a significant increase in the rate of bone loss following menopause for a period of 5-7 years after which the rate levels off. By the time women reach 80 years of age they have lost up to 40% of their peak bone mass. For men the lifetime loss of peak bone mass is around 25% and is a relatively steady decline, however, the rate of loss accelerates after 70 years of age.
The key factor is to build bone mass in childhood prior to reaching skeletal maturity (25 years of age). We should aim to have the best peak bone mass possible at 30 years of age in order to offset the natural decline in bone density over our lifetime.
Healthy bones are stronger than osteoporotic bones and can withstand more force and loading without suffering injury, and they will heal faster too
Where are the Common Fracture Sites of Osteoporosis and How Do They Happen?
Fractures caused by osteoporosis most often occur in the spine, hip, wrist and forearm. “Fragility” fractures occur from seemingly minor incidents such as falling down. In more serious cases, even coughing or sneezing can cause fractures.
Who is at Risk of Osteoporosis or Osteopenia?
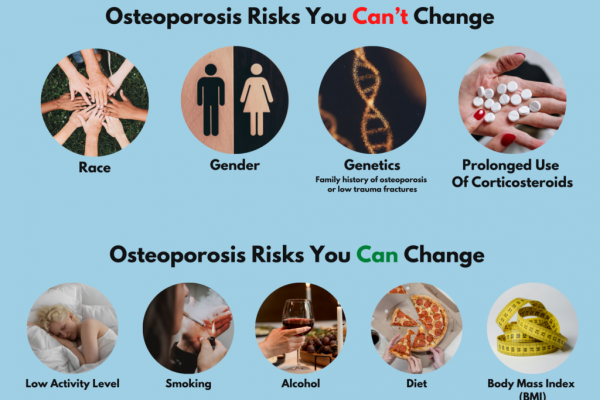
There are many risk factors which can increase your chances of suffering from osteoporosis – some we can’t change – for example genetics – if either of your parents have been diagnosed with osteoporosis, gender, race or previous use of steroids. Then there are some risks we can change – inactivity, smoking, drinking more than 2 units of alcohol daily and a diet low in calcium.
To determine your risk of breaking a bone, please visit the Healthy Bones Australia website and fill out this questionnaire
How is Osteoporosis Diagnosed?
To diagnose osteoporosis and assess your potential risk of fracture, you can have a scan which measures your Bone Mineral Density (BMD). It is most commonly performed using a dual-energy x-ray absorptiometry scan (DXA). It is a quick and painless test and there is a very low level of radiation.
The measurements, known as T-scores, can tell us if you have osteoporosis, osteopenia or normal bone density.
Preventing Osteoporosis and Osteopenia
While there are risk factors of osteoporosis that we cannot change (genetics, age), it is not completely out of our control. Making certain lifestyle changes can help you to reduce your risk of developing osteopenia or osteoporosis, or manage the condition if it has already been diagnosed.
Here we share several pathways you can take to preserve or even improve your bone density. Some or all may be relevant to you.
1. Medication
If you are have been diagnosed with osteoporosis then your Doctor may suggest that you start on a course of medication. Your Doctor is the best person to discuss which medication is best for you and to help you understand the pros and cons. Broadly speaking the medication either stimulates bone production (builds up bone) or as in the majority of medications, suppresses bone resorption (decreases the loss of bone).
2. Diet
A healthy balanced diet that includes Calcium, Vitamin D and Vitamin K as well as protein is recommended for improved bone health.
As bone is mostly made up of Calcium Phosphate, increase your intake of calcium rich foods such as milk, eggs and cheese. Remember that caffeine increases calcium loss so when combined with a diet low in calcium this has the potential to adversely affect your bone health.
Vitamin D helps the bone absorb calcium. A minimum of 10 minutes sun exposure on exposed skin in summer and 20 minutes in winter is recommended. Vitamin K is also important as it helps to make sure that calcium is deposited into the bones rather than into the soft tissue or organs.
Protein is essential for optimal bone mass gain during childhood and adolescence and also for preserving bone and muscle mass with aging.
A nutritionist or dietician is the best person to assist you in finding bone healthy foods that you enjoy eating. They may also advise you to take Calcium, Vitamin D or K supplements and what dosage is appropriate to improve your bone health.
3. Digestive Health
Your diet may be balanced but if your ability to absorb the nutrients is suboptimal then you are at risk. Speak with your doctor about your digestive health.
4. Lifestyle & Behavioral Changes
Smoking and alcohol consumption both have detrimental effects on bone health. Smoking is associated with lower bone mineral density, which can be attributed to factors such as disrupted bone turnover, earlier onset of menopause, lower body weight, and estrogen breakdown. On the other hand, alcohol consumption is linked to poor bone health and an increased risk of fractures. Alcohol interferes with calcium absorption and disrupts the production of hormones that are essential for maintaining strong bones. Both smoking and excessive alcohol intake should be minimised to promote optimal bone health.
5. Exercise – Our focus at Bone Health Asia

Bones thrive on physical loading and mechanical stress in order to tip the balance of bone remodelling in favour of deposition of new bone. The key is for the exercises to be weight bearing.
Exercise can help improve bone health but not all exercise is created equal. There are certain types of exercise that are beneficial for individuals with osteoporosis.
Our Bone Health Asia physiotherapists at Prohealth Sports And Spinal are licensed to safely deliver the Onero Programme, a research-based exercise programme that is specifically designed to prevent osteoporotic fracture by stimulating bone development and preventing falls. It is appropriate for adults of any age with osteoporosis and those who are at risk of developing it.

The Onero Bone Health Exercise programme is available at Prohealth Sports & Spinal's Wellington Street clinic
Onero means to “load” or “burden” in Latin and this is what is required to stimulate bone so as to maintain or improve our bone density. The Onero program consists of highly targeted exercises with high intensity loads and impact training.
Why is Supervised Exercise Beneficial for Bone Health and Density?
Bone loading exercises need to be done in a specific way and to be done safely, you need close supervision from health providers who have specific training.
The most important aspects of Onero TM are the following:
- How you lift: The way you move ensures that the load is transferred to the areas which need it the most.
- How much you lift: The weight has to be of a sufficient amount so as to stimulate the bone and strengthen muscles.
- Progression of load: The speed of progression is important to ensure safety.
What to expect in an Onero Bone Density Session?
The initial session involves a detailed assessment of your general health as well as understanding your specific bone health risk factors. We also conduct tests for balance, strength and flexibility. These measurements along with your bone scan results will dictate the starting point and speed of your progression on the programme.
In each 40 minute treatment session you will perform different types of “lifts” with varying loads, impact training, balance work and other specific exercises that are prescribed for you.
How does the Onero Bone Density Programme help with Bone Health?
Bone growth is slow. It takes at least 6 months for new bone to be laid down and the imaging results lag even further behind. Research results have shown that Onero TM helps both men and women with low to very low bone mineral density. The results have shown significant increases in bone mineral density, muscle strength, and balance as well as a decreased number of falls after a period of 8 months of training.
How Often Do I Need to Attend Sessions?
The original study which Onero is based upon, took a group of individuals with low to very low bone density and put them through training for 30 minutes 2 times a week over an 8 month period. Bone production and resorption never stops so you must continue to load your bones. After our peak bone mass is achieved, our bone density tends to decline with age. So, the old saying is true – if you don’t use it – you will lose it!
Learn More About The Onero Programme
Onero™ at Bone Health Asia located at Sports And Spinal Physiotherapy Centres provides one-on-one sessions, delivered by our clinically trained physiotherapists, driving you to better bone health. Our clinic is the first one in Asia that is licensed to safely deliver the Onero™ programme.
Any Questions? Reach Out To Us!
If you have any questions at all, please contact our clinic.
References
- Watson SL, Weeks BK, Weis L, Horan SA, and Beck BR (2015) Heavy resistance training is safe and improves bone, function and stature in postmenopausal woman with low to very low bone mass: Novel early findings from the LIFTMOR trial. Osteoporosis International, 2015, DOI 10.1007/s00198-015-3263-2.
- Beck BR, Weeks BK, Weis LJ, Harding A, Horan S, Watson SL: Restoring Standing Height: Yet Another Benefit of Exercise for the Osteoporosis. ASBMR 2015 Annual Meeting, Seattle, Washington, USA, Oct 9-12, 2015.
- Resource: The Chinese University of Hong Kong Jockey Club Centre for Osteoporosis Care and Control.
- Resource: International Osteoporosis Foundation (IOF).
- Resource: Healthy Bones Australia.
Written By

Judith Anne Gould
BPhty (Hons) (AUS) | MPhil (HK) Registered Physiotherapist (HK & AUS)
Judith has dedicated the majority of her physiotherapy career on assessing and treating dysfunctional posture and movement patterns through rehabilitation exercise and ergonomic intervention.
Having observed a high rate of osteoporosis conditions among her clients, Judith researched all the treatment options were available around the world. During that search, she came across LIFTMOR, a study which proved substantial improvement in the bone density through a targeted exercise programme. Judith became one of the first physiotherapists in Asia to complete the OneroTM Academy Programme.
She is passionate in educating patients to empower them to take charge of their own health. With OneroTM she hopes to show people that they can improve their bone health safely and effectively through exercise based treatment.